 |
 |
- Search
| Ann Child Neurol > Volume 32(1); 2024 > Article |
|
Abstract
Purpose
Idiopathic intracranial hypertension (IIH) is a clinical syndrome that mimics brain tumors with increased intracranial pressure. The present study is designed to investigate the diagnostic criteria of magnetic resonance imaging (MRI) and the severity of cerebrospinal fluid (CSF) pressure to understand the relationship and frequency of these criteria with the level of CSF pressure.
Methods
The present cross-sectional study was conducted on children diagnosed with IIH between the years 2011 and 2020, who were admitted to the pediatric neurology department of Ghaem Hospital, Mashhad, Iran. Clinical manifestations and imaging findings of the patients were recorded through a checklist.
Results
Forty-nine patients were included in the study; 27 (55.1%) were male, and 22 (44.9%) were female. The average CSF pressure was 40.64±20.63 cmH2O. The mean diameter distension of the perioptic subarachnoid space was 6.02±1.21 mm. Six (10.8%) patients had unilateral transverse sinus stenosis with an average CSF pressure of 20.47±36.80 cmH2O and 11 (21.4%) patients had bilateral transverse sinus stenosis with an average pressure of 48.22±21.04 cmH2O. In 22 (44.89%) patients, flattening of the posterior globe with the CSF pressure of 48.80±17.94 cmH2O was reported. Twenty-four (49%) patients had optic nerve tortuosity, with an average CSF pressure of 46.52±20.33 cmH2O. Among the diagnostic criteria, the pressure had a significant relationship with the flattening of the posterior globe (P<0.022).
Idiopathic intracranial hypertension (IIH) is a condition of increased intracranial pressure (ICP) with no laboratory or radiologic evidence of associated infection, space-occupying lesion, vascular abnormality, or hydrocephalus [1]. Although the pathophysiology of IIH is not entirely understood, either an increase in cerebrospinal fluid (CSF) production or a decrease in the absorption of CSF could lead to IIH [2]. Dysregulation of CSF dynamics and raised venous sinus pressure may be linked to pathophysiologic mechanisms of IIH. Furthermore, the link between IIH and obesity and female sex has given rise to theories that metabolic and hormonal factors may play a role [3].
IIH patients usually present with transient visual obscurations, headache, visual loss, and pulsatile tinnitus [1]. Clinical characteristics of IIH encompass non-specific new onset headache, papilloedema, and visual disturbances. Additionally, sixth nerve palsy may be present [4].
Despite an equal incidence of IIH between males and females before puberty, women comprise 90% of IIH cases above the age of 18 [5]. Although the national institute of health considers IIH a rare disorder with an estimated incidence of 0.9/100,000 annually worldwide, statistics indicate that the prevalence of IIH is likely to increase due to the obesity epidemic and advances in diagnosis [1,6,7]. Hence, it is recommended to manage IIH by losing weight, along with other treatments, including lumbar puncture, medication therapy, and surgery [1].
The diagnostic criteria of IIH are progressively moving from symptom-based standards to more quantifiable criteria. The most recent proposal advanced by Friedman et al. [8] is consistent with the widely accepted practice of setting lumbar puncture opening pressures at or above 25 cm CSF for adults of normal weight and 28 cm CSF or higher for children. They include magnetic resonance imaging (MRI) scan findings that are compatible with raised ICP. In addition, it has been recognized that IIH may present without symptoms of elevated ICP and exceptionally without papilloedema, commonly referred to as IIH without papilloedema [8].
Although the diagnosis of IIH can be executed by physical examination and medical history, imaging is applicable for better distinguishing whether the IIH is primary or secondary. The role of MRI in IIH is to rule out other disorders, detecting a secondary cause or the severity of the IIH. The following are MRI findings that are associated with IIH: an empty or partially empty sella turcica, perioptic subarachnoid space (SAS) distension, optic nerve protrusion, optic nerve tortuosity, slit-like ventricles, posterior aspect of the optic globe flattening, and transverse sinus stenosis [8,9].
Therefore, in this retrospective cross-sectional study, we evaluate the diagnostic criteria found in the MRI of young IIH patients and its relation with the CSF pressure levels of IIH patients.
In this retrospective study, by referring to the Ghaem Hospital's archives, we collected the files of children between 1 and 18 years diagnosed with IIH between 2011 and 2020 who were hospitalized in the pediatric neurology department of Ghaem Hospital in Mashhad. A pediatric neurologist confirmed the diagnosis of this disease. The diagnosis was made using proposals suggested by Friedman et al. [8] and Friedman and Jacobson [10], which are defined by high ICP along with normal brain parenchyma, in the absence of ventriculomegaly, mass lesion, underlying infection, or malignancy. All MRI were performed on a 1.5 Tesla system (Siemens, Munich, Germany) and included brain MRI (axial, sagittal and coronal T1 and T2; coronal T2 fat-saturated, fluid-attenuated inversion recovery [FLAIR], diffusion-weighted imaging, and apparent diffusion coefficient sequences), Magnetic resonance venography and orbital MRI (axial, sagittal and coronal T1 and T2, coronal T2 fat-saturated, and FLAIR sequences).
The necessary information was prepared and collected by a checklist. Our checklist contained the following parameters: gender, age, stenosis of the transverse sinus, distension of the perioptic SAS, flattening of the posterior globe, partial or complete empty sella turcica, optic nerve tortuosity, and CSF pressure.
Optic nerve tortuosity can be inferred when a complete visual of the nerve path is not possible in a single cut of a standard orbit axial MRI. Stenosis of the transverse sinus is defined as a change of caliber in the sinus from its origin to its termination. The determination of flattening of the posterior globe was made based on the straightening and loss of the normal outwards convexity of the sclera at the region of attachment to the optic nerve.
To examine complete or partial empty sella turcica, we employed the subsequent reporting system, classification, and scoring. Images of the empty space of the sella turcica were examined from the T1 view and mid-sagittal sections [11].
(1) Category 1: Normal
(2) Category 2: Slight upward concavity of the pituitary gland (the empty space of the sella turcica is less than one-third of the total height of the sella turcica)
(3) Category 3: The average upward concavity of the pituitary gland (the empty space of the sella turcica is between one-third and two-thirds of the total height of the sella turcica)
(4) Category 4: Severe upward concavity of the pituitary gland (the height of the empty space of the sella turcica is more than two-thirds of the total height of the sella turcica)
(5) Category 5: Pituitary tissue is not evident in the cavity of sella turcica.
Distension of the perioptic SAS is a subjective or objective finding with a different cut-off depending on the age. However, optic nerve sheath diameter >5.30 mm can be considered the cut-off for the distension of the perioptic SAS in all ages [12,13]. Fig. 1 illustrates examples of characteristic MRI findings observed in IIH.
Our inclusion criteria were an age range between 1 and 18 years and a diagnosis of IIH based on clinical and MRI evidence. The criteria for exclusion were if 50% of pertinent information was inaccessible or if the patient received a diagnosis of secondary IIH.
After collecting the data, all the data were entered into SPSS software version 28 (IBM Co., Armonk, NY, USA). Central and dispersion indicators described quantitative variables, and qualitative variables were described by frequency and frequency percentage. In order to analyze the data, independent and post hoc t-test and analysis of variance (ANOVA) test were used. In all studies, the significance level was considered less than 0.05. GraphPad Prism version 9 software (GraphPad Software Inc., San Diego, CA, USA) was used to draw graphs.
The information of the participants was kept confidential. Personal information, including names and surnames, was not recorded in the software; instead, each person was assigned a unique project-specific code for the analysis. This study was approved on the 3rd of March 2021 by the Mashhad University of medical sciences ethical committee with the ethics committee number 1398.085.IR.MUMS.MEDICAL.REC. Written informed consent by the patients was waived due to a retrospective nature of our study.
After examining the cases, 49 cases were included in the study, and the results of data collection and analysis are as follows.
The results of examining the files showed that 27 (55.1%) of the 49 patients were male, and 22 (44.9%) were female (Table 1). The data analysis showed that the minimum age was 1 year, the maximum age was 16, and the average age in total patients was 8.3±3.75 (Table 1). Also, the mean±standard deviation of the recorded CSF pressure was 40.64±20.63 cmH2O (Table 1). In addition, the minimum distension of the perioptic SAS was 3.20 mm, the maximum was 9.90 mm, and its mean±standard deviation was 6.02±1.21 (Table 1).
Table 2 discusses the stenosis of the transverse sinus. Seventeen patients were diagnosed with stenosis of the transverse sinus. Of these, 11 (21.4%) patients had bilateral transverse sinus stenosis with a mean pressure of 48.22±21.04, and six (10.8%) had unilateral stenosis of the transverse sinus with a mean pressure of 36.80±20.47 cmH2O. A comparison of mean CSF pressure in the four groups showed no significant difference. Despite a 5 cmH2O pressure differential between patients with and without transverse sinus stenosis, no significant difference was observed in statistical analysis (P=0.578).
Data analysis also revealed that posterior globe flattening was reported in 22 (44.89%) patients with an average CSF pressure of 17.94±48.80 cmH2O. Additionally, the comparison between the two groups demonstrated a marked difference in CSF pressure, with individuals presenting posterior globe flattening having a significantly higher pressure compared to those without it (P<0.05) (Table 2).
The results related to the findings of complete or partial empty sella turcica showed that out of a total of 49 patients, 11 (22.4%) patients were in category 1, 12 (24.5%) were in category 2, 17 (34.5%) were in category 3, three (6.1%) patients in category 4, and six (12.2%) were not evaluable. Also, no significant difference was observed in the overall comparison between the groups (P=0.061) (Table 2).
In addition, a post hoc test was used to compare each group. The results indicated that category 1 and 2 were at the threshold of significance in the CSF pressure (P=0.058), whether category 3 patients had significantly higher CSF pressure compared to category 1 (P<0.01) (Fig. 2).
Regarding the criterion of optic nerve tortuosity, the data analysis showed that out of the total number of patients, 24 (49%) had optic nerve tortuosity with average CSF pressure of 46.52±20.33 cmH2O. In comparing the two groups in which optic nerve tortuosity could be assessed, no significant difference was observed between the two groups in terms of mean CSF pressure (P=0.090) (Table 2).
IIH is a medical condition characterized by elevated ICP in the absence of any clinical, laboratory or radiological evidence of an intracranial space occupying. Due to the incorrect assumption that IIH is a rare condition in children, many practitioners rarely consider it in the differential diagnosis. The reason for concern is that if IIH is left untreated, it can lead to poor quality of life and various morbidities, including vision loss [14-16].
To our knowledge, no similar study was published on children; therefore, the results of the present study were compared with those of similar studies on adults. According to prior studies, the most common neuroimaging sign in IIH is posterior globe flattening, followed by complete or partial empty sella turcica and optic nerve tortuosity [17,18]. In addition, Prabhat et al. [18] used several imaging criteria to assess the prevalence and accuracy of predicting the diagnosis of IIH. Eighty untreated patients with IIH and 30 control patients with a mean age of 30.91 years were selected according to a predefined criterion. The results showed that the most common abnormality observed was tortuosity of the optic nerve (82.5%), followed by flattening of the posterior globe (80%), distension of the perioptic SAS (73.8%), and complete or partial empty sella turcica (68.8%). The tortuosity of the optic nerve was identified as the most sensitive sign on neuroimaging, while the flattening of the posterior globe and distension of the perioptic SAS displayed the highest specificity. It has been stated that more than three neuroimaging features are linked to the intensity of vision loss [18].
Another case-control study in pediatrics showed that transverse venous sinus stenosis has a sensitivity of 74% and specificity of 100% in diagnosing IIH. It also indicated that flattering of the posterior globe and transverse sinus stenosis are significantly found in IIH patients compared to controls. Additionally, the presence of one of the three criteria (transverse sinus stenosis, flattening of posterior globe, or pituitary gland flattering) in patients has the sensitivity of 65% and specification of 95% for diagnosing IIH. This study has also proposed the importance and upsides of MRI in diagnosing IIH [19].
Although the exact mechanism for IIH is unclear, some thesis has been proposed. Previously hypersecretion of CSF was known to be the leading theory in the pathophysiology of IIH. In contrast, it has been demonstrated that excessive CSF secretion due to causes such as choroid plexus hyperplasia can result in ventriculomegaly and hydrocephalus, unlike IIH, where we observe normal or reduced ventricular size [20,21]. Another mechanism that could lead to IIH is the impairment in resorption of CSF because of various causes, such as cerebral venous stenosis. Cerebral venous stenosis can cause impairment in the resorption of CSF by decreasing venous overflow and accumulation of CSF. However, as our study and other studies confirm, there is no association between CSF opening pressure and the degree of stenosis [22]. Lastly, obesity is historically considered part of the IIH pathogenicity due to the interleukin and cytokine role and the pressure that obesity puts on the heart, causing decreased venous return [22].
Our findings also demonstrated that category 3 of complete or partial empty sella turcica proved to have higher CSF pressure than category 4. Although it is acknowledged that empty sella is a common reported imaging finding in patients with IIH, but it is also quite common in the general population and it has been reported as an incidental radiologic finding in healthy subjects, exhibiting the same characteristic as in IIH patients. So this finding can be because the complete or partial empty sella turcica can exist as a normal variant in individuals, and the decrease in the average CSF pressure in this study does not distort the present results [13,23,24].
The research had certain limitations, including the fact that the sample only included patients from the neurology department of Ghaem Hospital, and the sample size was small to make generalizations. In this retrospective and cross-sectional study, certain patient information was not recorded. The absence of a control group was noted as a limitation.
Our study on MRI diagnostic criteria unveiled a significant correlation between CSF pressure and the posterior globe flattening. Conversely, a similar study on adults showed a weak positive correlation between CSF opening pressure and bilateral transverse sinus stenosis on MRI [25]. The cause of these differences is unknown. Given the lack of prior research in this specific field in pediatrics, it is recommended that further studies be conducted across multiple centers and with a larger cohort of patients to establish a more comprehensive relationship between MRI diagnostic criteria and CSF pressure in pediatric patients with IIH. The present study examined the diagnostic features of MRI in IIH patients and reported the frequency of each of these features for disease diagnosis. Given that MRI is a non-invasive modality for evaluating IIH patients, and some patients are disinclined to undergo invasive procedures, such as lumbar puncture, the findings of this study may aid in diagnosing and monitoring these patients. The utilization of neuroimaging findings in patients with IIH could prove beneficial in the early prediction of CSF pressure and risk stratification for diagnosis of IIH.
Notes
Author contribution
Conceptualization: FST, JA, FA, MBT, NT, and NH. Data curation: FST, JA, FA, MBT, SI, AK, EHN, AP, and NH. Formal analysis: BB, YS, SI, EHN, AP, and AMG. Methodology: SI, EHN, AP, NT, AMG, and NH. Project administration: NH. Visualization: YS, MBT, SI, EHN, NT, and NH. Writing-original draft: BB, FST, YS, AK, EHN, AP, NT, and AMG. Writing-review & editing: FST, FA, MBT, SI, EHN, AP, AMG, and NH.
Acknowledgments
The authors would like to express their gratitude for the collaboration provided by Mashhad University of Medical Sciences.
Fig. 1.
Characteristic magnetic resonance imaging findings in idiopathic intracranial hypertension. (A, B) Distension of the perioptic subarachnoid space. (C) Optic nerve tortuosity. (D) Flattening of the posterior globe. (E) Stenosis of the left transverse sinus. (F) Empty sella turcica.
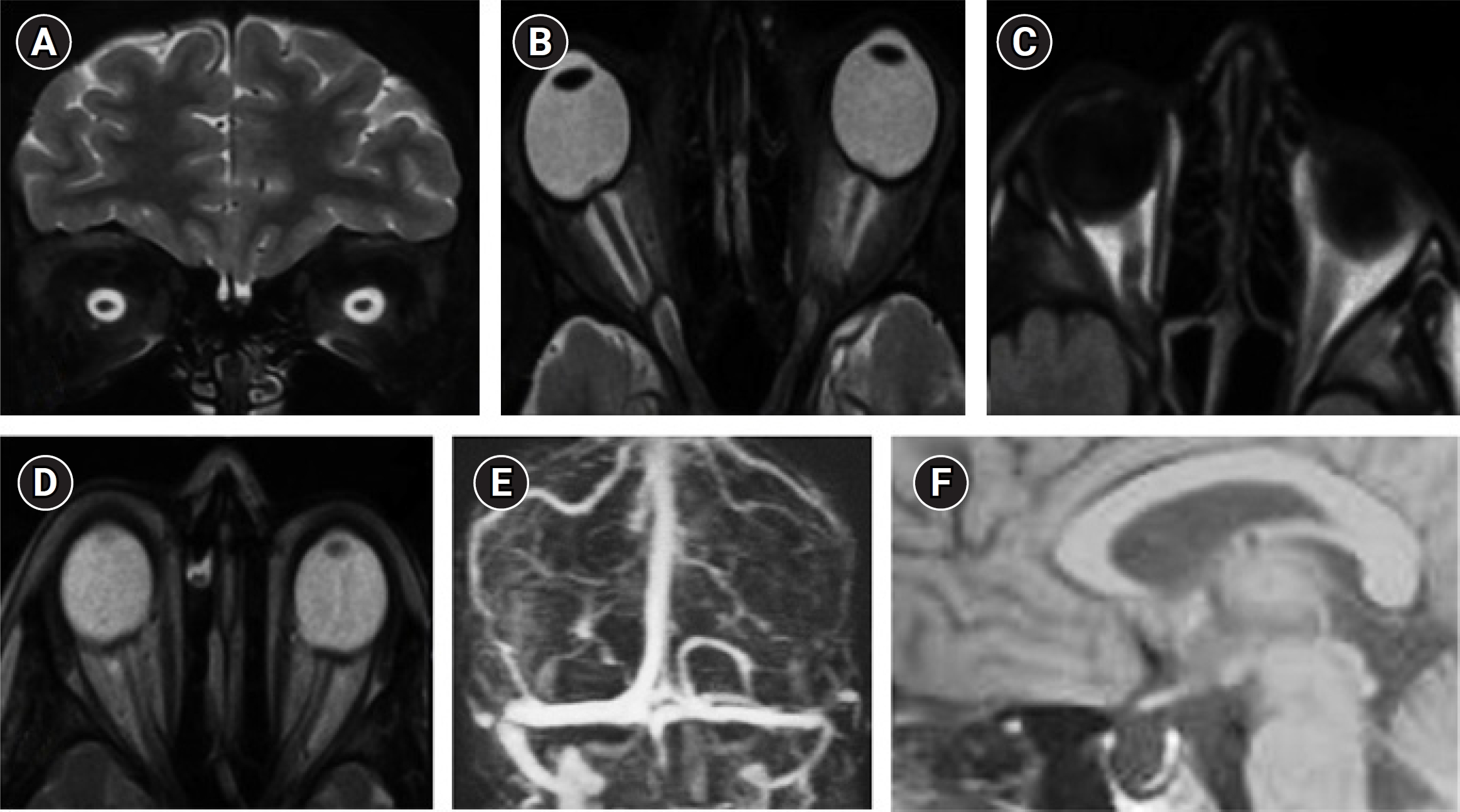
Fig. 2.
Comparison of groups in terms of cerebrospinal fluid (CSF) pressure compared to category 1. Data are presented by mean±standard deviation. aP<0.01.

Table 1.
Demographic data and CSF pressure of the examined patients
Table 2.
Magnetic resonance imaging presentations in the examined patients
References
2. Johnston I. The definition of reduced CSF absorption syndrome: a reappraisal of benign intracranial hypertension and related conditions. Med Hypotheses 1975;1:10-4.


3. Wang MT, Bhatti MT, Danesh-Meyer HV. Idiopathic intracranial hypertension: pathophysiology, diagnosis and management. J Clin Neurosci 2022;95:172-9.


4. Wakerley BR, Mollan SP, Sinclair AJ. Idiopathic intracranial hypertension: update on diagnosis and management. Clin Med (Lond) 2020;20:384-8.



5. Portelli M, Papageorgiou PN. An update on idiopathic intracranial hypertension. Acta Neurochir (Wien) 2017;159:491-9.



6. Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri: population studies in Iowa and Louisiana. Arch Neurol 1988;45:875-7.


7. Jacobs D, Corbett J, Balcer L. Annual incidence of idiopathic intracranial hypertension (IIH) in the Philadelphia area. Paper presented at the 13th Annual Meeting of the North American Neuro-Ophthalmology Society; 2004 Mar 27-Apr 1; Orlando, FL.
8. Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 2013;81:1159-65.


9. Barkatullah AF, Leishangthem L, Moss HE. MRI findings as markers of idiopathic intracranial hypertension. Curr Opin Neurol 2021;34:75-83.



10. Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology 2002;59:1492-5.


11. Yuh WT, Zhu M, Taoka T, Quets JP, Maley JE, Muhonen MG, et al. MR imaging of pituitary morphology in idiopathic intracranial hypertension. J Magn Reson Imaging 2000;12:808-13.


12. Geeraerts T, Newcombe VF, Coles JP, Abate MG, Perkes IE, Hutchinson PJ, et al. Use of T2-weighted magnetic resonance imaging of the optic nerve sheath to detect raised intracranial pressure. Crit Care 2008;12:R114.



13. Saindane AM, Lim PP, Aiken A, Chen Z, Hudgins PA. Factors determining the clinical significance of an “empty” sella turcica. AJR Am J Roentgenol 2013;200:1125-31.


14. Rangwala LM, Liu GT. Pediatric idiopathic intracranial hypertension. Surv Ophthalmol 2007;52:597-617.


15. Aylward SC, Way AL. Pediatric intracranial hypertension: a current literature review. Curr Pain Headache Rep 2018;22:14.



16. Aylward SC. Pediatric idiopathic intracranial hypertension: a need for clarification. Pediatr Neurol 2013;49:303-4.


17. Manfre L, Lagalla R, Mangiameli A, Lupo F, Giuffre G, Ponte F, et al. Idiopathic intracranial hypertension: orbital MRI. Neuroradiology 1995;37:459-61.



18. Prabhat N, Chandel S, Takkar DA, Ahuja C, Singh R, Kathirvel S, et al. Sensitivity and specificity of neuroimaging signs in patients with idiopathic intracranial hypertension. Neuroradiol J 2021;34:421-7.




19. Kohli AA, Vossough A, Mallery RM, Woo JH, Sheldon CA, Paley GL, et al. Magnetic resonance imaging findings in pediatric pseudotumor cerebri syndrome. Pediatr Neurol 2019;99:31-9.



20. Baykan B, Ekizoglu E, Altiokka Uzun G. An update on the pathophysiology of idiopathic intracranial hypertension alias pseudotumor cerebri. Agri 2015;27:63-72.


21. Cleves-Bayon C. Idiopathic intracranial hypertension in children and adolescents: an update. Headache 2018;58:485-93.



22. Burkett JG, Ailani J. An up to date review of pseudotumor cerebri syndrome. Curr Neurol Neurosci Rep 2018;18:33.



23. Foresti M, Guidali A, Susanna P. Primary empty sella: incidence in 500 asymptomatic subjects examined with magnetic resonance. Radiol Med 1991;81:803-7.

- TOOLS







