|
 |
- Search
| Ann Child Neurol > Volume 32(1); 2024 > Article |
|
Mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes (MELAS) is a multisystem disorder mostly caused by mutations in mitochondrial DNA [1]. The pathogenic variant m.3243A>G accounts for more than 80% of cases of MELAS syndrome. The clinical manifestations of MELAS are highly diverse and include seizures, dementia, stroke-like episodes, migraines, depression, sensorineural hearing loss, muscle weakness, cardiomyopathy, and diabetes mellitus. Cortical blindness due to stroke-like episodes is another possible clinical manifestation [1]. Here, we describe the case of a patient with MELAS with the m.3243A>G pathogenic variant who visited our hospital with symptoms of bilateral total visual loss. We treated this patient with high-dose dexamethasone, and the patient recovered almost completely from visual loss.
A 15-year-old boy with no remarkable perinatal history and no family history of stroke presented to our emergency department with aphasia, paraphasia, acalculia, right-to-left disorientation, and finger agnosia. Brain magnetic resonance imaging (MRI) and magnetic resonance angiography were performed, and an acute left middle cerebral artery infarct was suspected. Initial electroencephalography demonstrated persistent left hemispheric slowing with fluctuating amplitude. The initial lactate level was mildly elevated, at 2.8 mmol/L. Although bilateral sensorineural hearing loss had developed after 3 years and the patient wore hearing aids thereafter, the initial evaluation of hearing, echocardiography, and electrocardiography showed no abnormal findings. He was administered oral levetiracetam to prevent seizures. However, 5 days later, he developed generalized tonic-clonic seizures. The oral levetiracetam dose was increased from 1,000 mg/day in 2 divided doses to 1,500 mg/day in 2 divided doses. The patient was discharged after remaining seizure-free for 2 days. After another 3 days, his right hand became immobile, and a headache began and worsened, resulting in re-admission. Suspecting a new stroke-like episode, evaluation for MELAS was performed, including a mitochondrial DNA test. A pathogenic variant of m.3243A>G (heteroplasmy, 53%) was detected, and the patient was diagnosed with MELAS. Subsequently, he received conservative care to monitor his blood glucose levels and prevent seizures. Within less than a year from this event, the patient was diagnosed with diabetes mellitus.
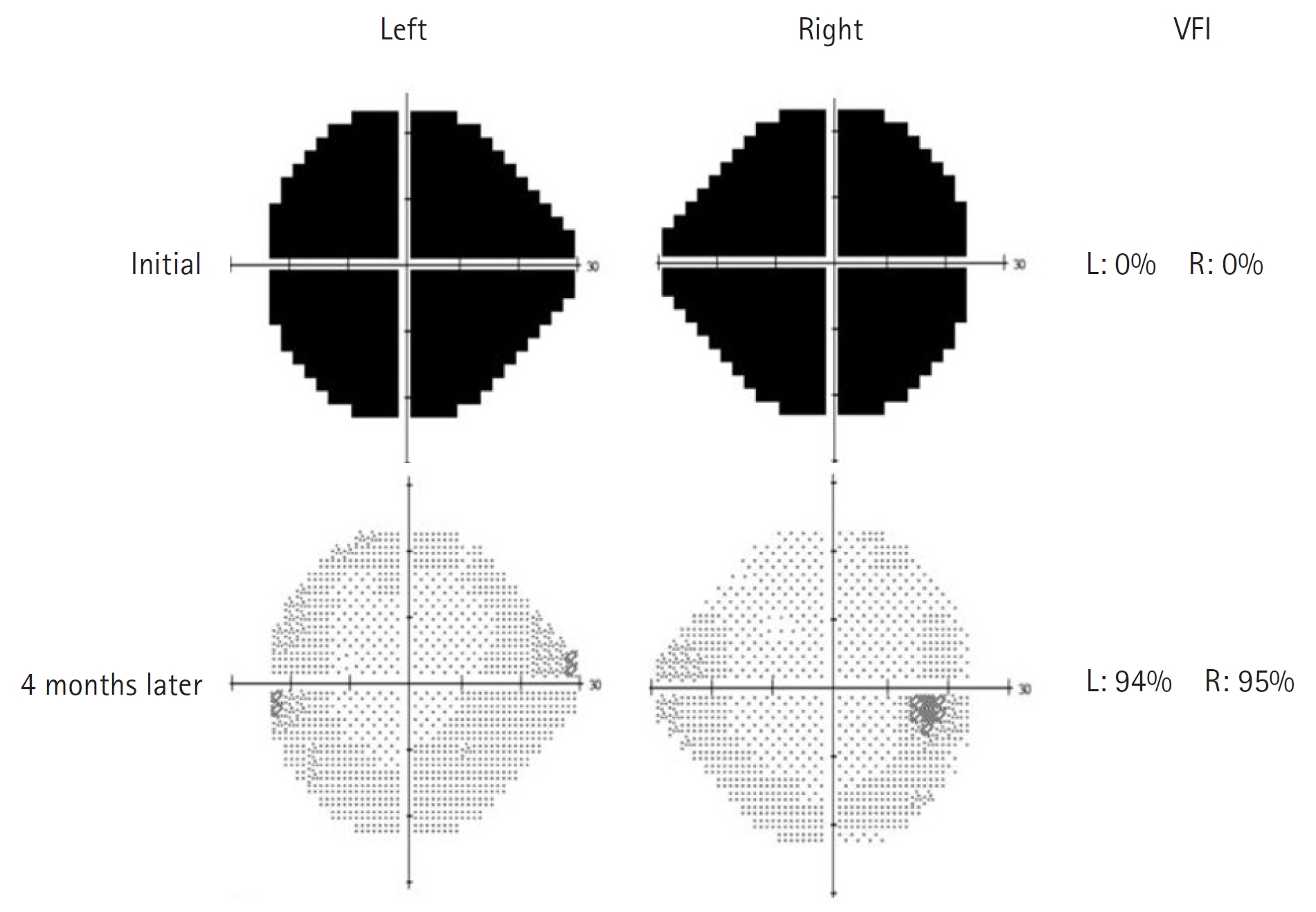
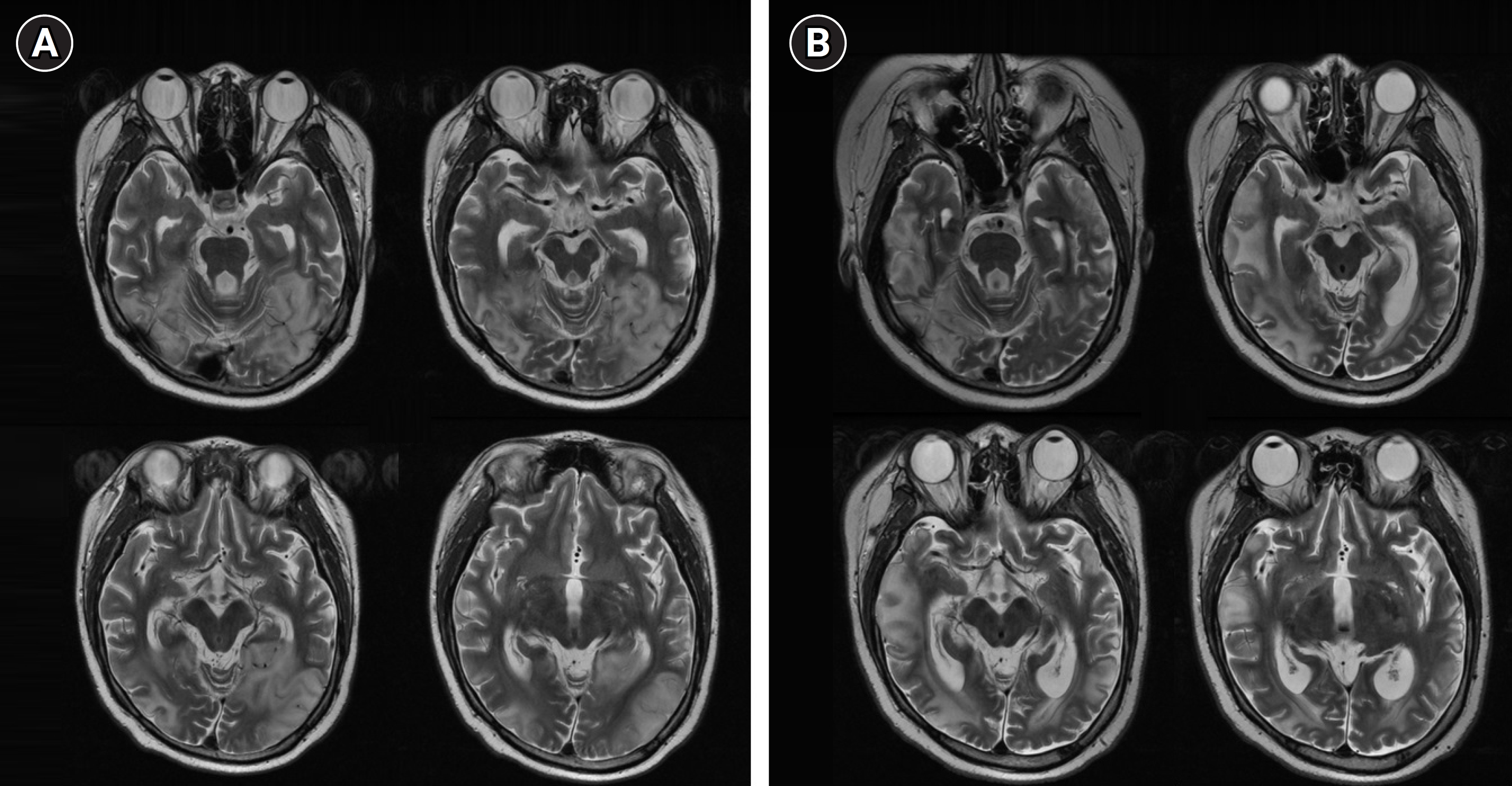
Two years later, he was readmitted to our hospital because of headache and visual disturbance at 17 years of age. Brain MRI and magnetic resonance spectroscopy showed progression of MELAS. Newly developed lesions simultaneously invading the cortical gray matter and subcortical white matter were observed in the parietal, temporal, and occipital areas (Fig. 1A). A visual field test revealed total visual loss in both eyes (Fig. 2). The serum lactate level was also measured at 8.1 mmol/L, which was four times the upper limit of the normal range. His headache with visual disturbance was judged to be indicative of MELAS progression, and high-dose dexamethasone (20 mg/body surface area [BSA]/day for 7 days followed by 10 mg/BSA/day for another 5 days) and mannitol treatment were initiated to stabilize the brain lesion. Intravenous arginine and anti-seizure medications were administered [2]. Gradually, the patient's visual disturbances began to improve, and the serum lactate level stabilized between 3 and 4 mmol/L. The steroid dose was gradually reduced further, and he was maintained on low-dose prednisolone (1 mg/kg/day, maximum 30 mg/day) and was discharged 1 month after the onset of symptoms. Four months after symptom onset, brain MRI showed improvement in both occipital areas, but newly developed high-intensity lesions at the right and left parieto-temporal lobes were also noted (Fig. 1B). The visual disturbance was almost completely resolved in a follow-up visual field test (Fig. 2). Afterward, the patient's visual disturbances and seizures waxed and waned; however, the frequency of symptom recurrence gradually but significantly decreased, making it easier to perform daily activities.
Stroke-like episodes in MELAS are distinguishable from ischemic stroke because they are often recurrent, slowly progressing events with damaged areas often observed in the cortex and subcortical white matter with relative sparing of the deep white matter [2,3]. During stroke-like episodes, these lesions often do not strictly adhere to the typical cerebrovascular territories observed in ischemic stroke [1]. These differences are believed to be due to the presence of distinct underlying pathogenic mechanisms. Mitochondrial angiopathy and cytopathy are considered two key features that drive the pathogenesis of stroke-like episodes in patients with MELAS [2-6]. Mitochondrial angiopathy is characterized by the proliferation of abnormally enlarged mitochondria in the endothelial and smooth muscle cells of the cerebral arterioles and capillaries [5]. Such vessels with impaired mitochondrial function are vulnerable to the dysregulation of blood flow owing to their vasodilatory effect, which eventually leads to vasogenic edema. Conversely, mitochondrial cytopathy results from mitochondrial metabolic dysfunctions, such as reduced glucose oxidation, increased glycolysis, increased lactate production, mitochondrial membrane potential fluctuations, and disrupted calcium homeostasis leading to cell death [2]. Furthemore, the sequence of dominant pathogenic mechanisms in play during stroke-like episodes is of interest. Vasogenic edema during stroke-like episodes on brain MRI is characterized by T2 hyperintensity, fluid-attenuated inversion recovery hyperintensity, and apparent diffusion coefficient (ADC) hyperintensity [4]. Several studies have proposed that vasogenic edema precedes cytotoxic edema, which is characterized by diffusion-weighted image hyperintensity and ADC hypointensity [4-6]. Accordingly, treatment of vasogenic edema may, at least in part, attenuate the extent of subsequent cytotoxic edema, leading to a favorable prognosis. High-dose steroid therapy has been administered to patients with MELAS during stroke-like episodes [6,7]. Although no clinical trials have been conducted, previous studies have reported the beneficial effects of high-dose treatment during stroke-like episodes [7].
Here, we describe a case of a patient who recovered from complete bilateral cortical blindness after high-dose dexamethasone therapy, which, to our knowledge, has not been published thus far and may serve as a reference case report for patients in similar clinical scenarios. We consider this case to be a rare therapeutic outcome in which bilateral total visual loss during stroke-like episodes in MELAS dramatically improved with high-dose steroid therapy. The protective effects of steroids, such as reduced inflammation, reactive gliosis, excitotoxicity, and oxidation, as well as decreased apoptosis, may have contributed to the patient’s recovery [8]. A recent report described vision loss due to ischemic optic neuropathy as the first presentation in a patient with MELAS, whose vision loss remained stable despite prednisone treatment (50 mg/day for 12 days) [9]. The different results between this study and our study might be due to the total steroid dose administered or different mitochondrial heteroplasmy rates of the involved tissues. Furthermore, little is known regarding the availability of effective treatment options for the cytotoxic edema seen on brain MRI scans of patients with MELAS following stroke-like episodes. Newer drugs, such as bumetanide, glibenclamide, and vasopressin receptor antagonists, may be viable options for the treatment of cytotoxic edema [10]. Whether a combination of steroid therapy targeting vasogenic edema and other drugs for cytotoxic edema further enhances the overall recovery process from stroke-like episodes is currently unknown and must be addressed in future studies.
This study was approved by the Institutional Review Board of the Gangnam Severance Hospital, Yonsei University College of Medicine (3-2022-0121). The requirement for informed consent for this retrospective study was waived by the board.
Conflicts of interest
Young-Mock Lee is an editorial board member of the journal, but he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Notes
Author contribution
Conceptualization: SJL, JHN, and YML. Data curation: SJL and JHN. Methodology: SJL, JHN, and YML. Visualization: SJL and JHN. Writing-original draft: SJL and JHN. Writing-review & editing: SJL, JHN, and YML.
Acknowledgments
The authors are grateful to all staff members, doctors, and statistical consultants involved in this study.
Fig. 1.
T2-weighted magnetic resonance imaging findings. (A) The initial T2 axial images reveal bilateral high signal intensity in the cortical gray matter and subcortical white matter of both parieto-temporo-occipital areas. (B) Four-month follow-up T2 axial images reveal progressive resolution of the bilateral high-intensity signals in the occipital areas, but newly developed high-intensity lesions at the right and left parieto-temporal lobes.
References
1. El-Hattab AW, Adesina AM, Jones J, Scaglia F. MELAS syndrome: clinical manifestations, pathogenesis, and treatment options. Mol Genet Metab 2015;116:4-12.


2. Koenig MK, Emrick L, Karaa A, Korson M, Scaglia F, Parikh S, et al. Recommendations for the management of strokelike episodes in patients with mitochondrial encephalomyopathy, lactic acidosis, and strokelike episodes. JAMA Neurol 2016;73:591-4.


3. Fryer RH, Bain JM, De Vivo DC. Mitochondrial encephalomyopathy lactic acidosis and stroke-like episodes (MELAS): a case report and critical reappraisal of treatment options. Pediatr Neurol 2016;56:59-61.



4. Yoneda M, Maeda M, Kimura H, Fujii A, Katayama K, Kuriyama M. Vasogenic edema on MELAS: a serial study with diffusion-weighted MR imaging. Neurology 1999;53:2182-4.


5. Bi WL, Baehring JM, Lesser RL. Evolution of brain imaging abnormalities in mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes. J Neuroophthalmol 2006;26:251-6.


6. Walcott BP, Edlow BL, Xia Z, Kahle KT, Nahed BV, Schmahmann JD. Steroid responsive A3243G mutation MELAS: clinical and radiographic evidence for regional hyperperfusion leading to neuronal loss. Neurologist 2012;18:159-70.


7. Finsterer J, Frank M. Glucocorticoids for mitochondrial disorders. Singapore Med J 2015;56:122-3.



8. Garcia-Segura LM, Balthazart J. Steroids and neuroprotection: new advances. Front Neuroendocrinol 2009;30:v-ix.