Hemiplegic migraine (HM) is a rare subtype of migraine with aura, characterized by the gradual progression of varying degrees of hemiparesis (motor aura) or other neurological deficits. HM has two forms: familial and sporadic. Sporadic HM (SHM) is defined as HM without a family history of similar episodes. Abnormalities in cerebral perfusion have been suggested as a potential cause of encephalopathy and hemiplegia in both SHM and familial HM (FHM).
Hyperperfusion is thought to be linked to the positive symptoms of migraine with aura, such as visual hallucinations, while hypoperfusion is associated with negative symptoms [1]. In contrast, hyperemia has been identified as the underlying pathophysiology of negative symptoms of HM, such as hemiplegia and encephalopathy [2]. Hyperperfusion in HM has been demonstrated using diffusion-weighted magnetic resonance imaging (DW-MRI), perfusion MRI, magnetic resonance angiography (MRA), and technetium-99m (99mTc) hexamethylpropyleneamine oxime (HMPAO)-single-photon emission computed tomography (SPECT) [3-5]. We present two cases of SHM, in an 18-year-old male patient and a 13-year-old boy. In these cases, the patients had SHM accompanied by contralateral cerebral hemispheric hyperemia, as observed on susceptibility-weighted imaging (SWI) and additional studies.
Informed consent was obtained from all parents. Patient medical records and other data were anonymized to ensure confidentiality.
1. Case 1
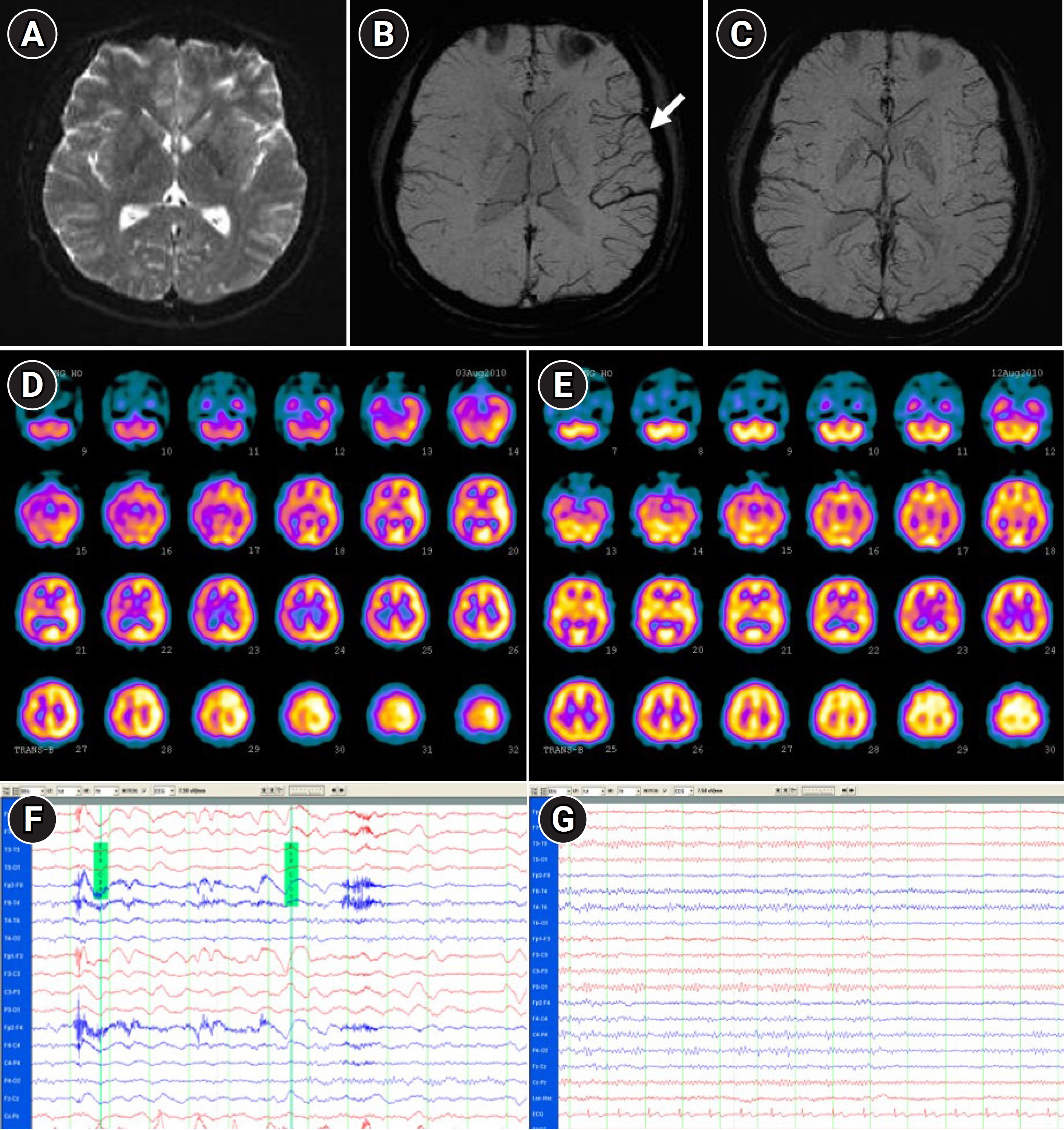
An 18-year-old male patient was admitted to the hospital with reports of headache, nausea, aphasia, right hemiparesis, and decreased mental status for 1 day. He had also been experiencing confusion and drowsiness. The patient had a history of recurrent right hemiparesis and encephalopathy since the age of 8 years. At 15 years old, he visited a university hospital for a similar episode. At that time, brain MRI and routine laboratory test results were normal. He visited our hospital with the same symptoms and underwent brain MRI and MRA, laboratory examinations, and cerebrospinal fluid (CSF) analysis, all of which yielded normal results. Initial electroencephalography (EEG) revealed diffuse cerebral dysfunction that normalized 3 days later. Two days after symptom onset, the patient fully recovered without any special treatment. No family members had a history of migraine with or without aura or HM. SHM was suspected, and propranolol was administered as prophylactic medication. Between episodes, the patient was healthy but experienced intermittent migraine attacks with aura. Three hours before the onset of the most recent attack, the patient reported discomfort in his right arm, a right-throbbing headache, nausea, and vomiting. On day 1 of the current hospital admission, neurological examination revealed aphasia, right hemiparesis, right-sided hypoesthesia, and right-sided hemineglect. Laboratory tests, including serum and urine chemistry, ammonia, thyroxine, triiodothyronine, thyroid-stimulating hormone, antinuclear antibody, and CSF analyses, revealed no notable abnormalities. We found no mutations in the CACNA1A gene on chromosome 19, the ATP1A2 gene on chromosome 1, or the SCN1A gene on chromosome 2. EEG showed generalized delta-to-theta wave slowing, predominantly over the left cerebral hemisphere (Fig. 1F). T1/T2 DW-MRI results were normal, while SWI revealed prominent vessels in the left hemisphere (Fig. 1A and B). On day 2, 99mTc-HMPAO-SPECT showed increased tracer uptake in the left cerebral hemisphere (Fig. 1D), which was consistent with the SWI findings (Fig. 1B). Nonsteroidal anti-inflammatory drugs, ondansetron, and metoclopramide were administered. On day 3, the patient’s mental status improved, but the left-sided headache persisted. We prescribed amitriptyline (40 mg daily) as prophylaxis for HM attacks. On day 7, the headache resolved, and the patient was discharged. Follow-up EEG on day 11 was normal (Fig. 1G). DW-MRI (T1/T2) with SWI (Fig. 1C) and 99mTc-HMPAO-SPECT (Fig. 1E) performed on day 11 did not reveal hyperemia in the left hemisphere, and no significant difference in perfusion was observed between the two cerebral hemispheres. Since then, the patient has been taking topiramate and has visited the emergency room approximately once a year, with reports of severe headache and hemiparesis.
2. Case 2
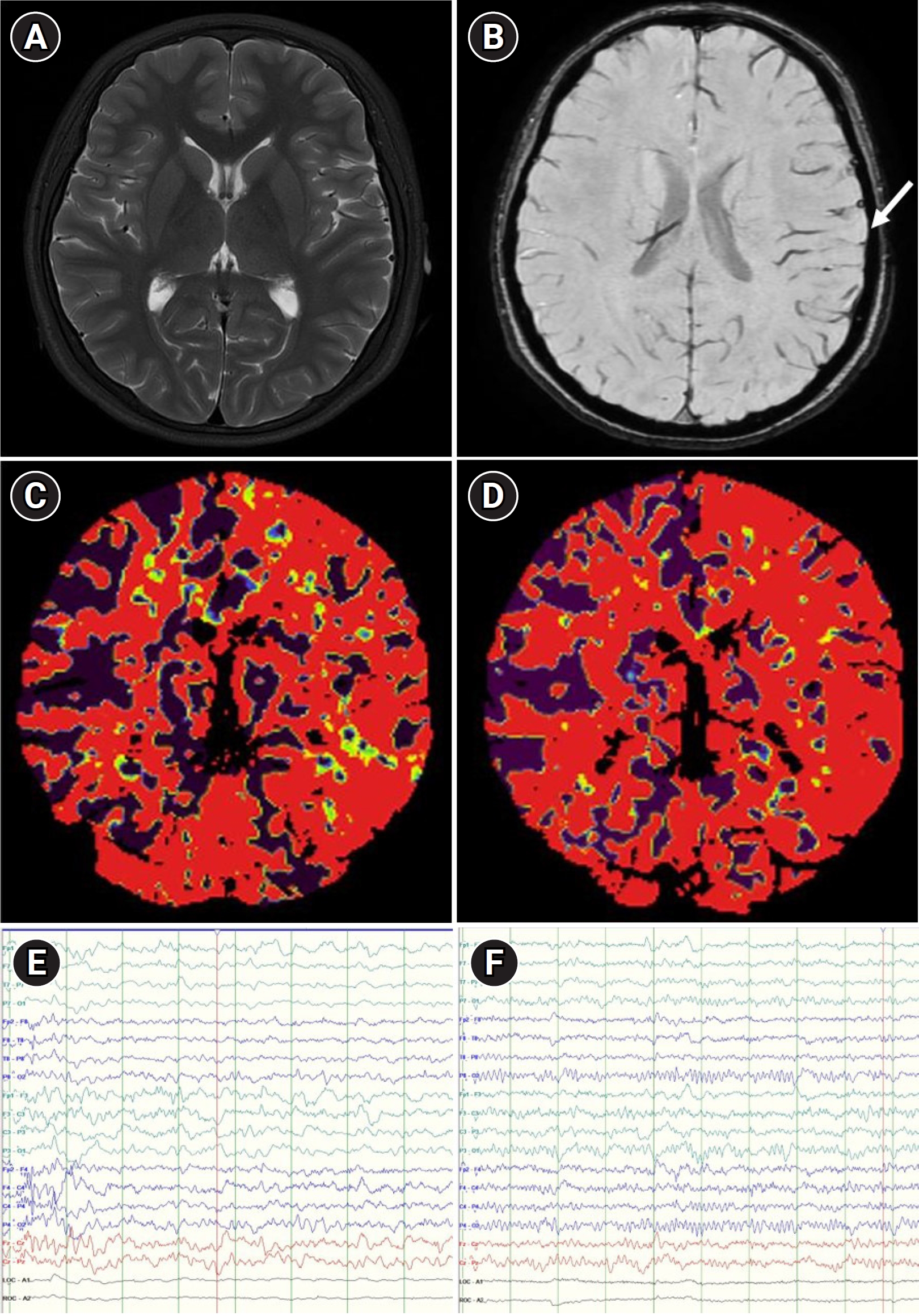
A 13-year-old male patient was admitted to the emergency room, presenting with motor weakness and numbness on the right side of his body, speech disturbances, and migraine. He had experienced two episodes of recurrent right hemiparesis, numbness, and headache since the age of 11 years. At that age, he first visited our emergency room with symptoms of headache, numbness, and slurred speech after being hit in the head by a ball. Computed tomography (CT) revealed no specific findings. All symptoms improved within 1 day of the hospital visit without any special treatment. Within 1 day of discharge, the patient reported headaches and a return of impaired verbal expression, accompanied by fever, and returned to the emergency room. Laboratory investigations, including CSF studies, EEG, and brain MRI, were performed to differentiate stroke from meningitis. Laboratory investigations, including CSF studies (involving autoimmune disease evaluations, such as adenosine deaminase, oligoclonal band, and immunoglobulin G tests), were within normal limits. EEG revealed left hemispheric dysfunction. The patient was treated for encephalitis, receiving antibiotics (vancomycin and cefotaxime), antiviral medication (acyclovir), and intravenous immunoglobulin (0.4 mg/kg) for 4 days, considering potential viral, bacterial, and autoimmune causes. However, all symptoms resolved within a day of hospitalization. The follow-up EEG was normal after symptom recovery, and encephalitis treatment was discontinued. The patient revisited the emergency room at 13 years old. As before, no specific findings were revealed by laboratory examinations or CSF analysis performed at this time. The EEG suggested left hemispheric dysfunction (Fig. 2E). DW-MRI results were normal (Fig. 2A), while SWI showed a marked dark signal in the cortical veins of the left cerebral hemisphere (Fig. 2B). CT perfusion imaging revealed increased cerebral blood volume and slightly increased cerebral blood flow in the left cerebral hemisphere (Fig. 2C and D), indicating increased oxygen demand in that hemisphere. All symptoms improved within 5 hours of symptom onset without special treatment. Follow-up EEG conducted the next day was normal (Fig. 2F). The patient’s mother also had migraines with aura. However, genetic mutations suggestive of FHM were not identified using diagnostic exome sequencing. Therefore, the patient was diagnosed with SHM and prescribed topiramate for headache control. After discharge, he experienced a single episode of hemiparesis and has reported numbness and headache lasting several hours about once a month.
SHM is on the spectrum of migraine with aura and shares clinical features with FHM. Like FHM, SHM is characterized as migraine with aura and includes motor weakness; however, in SHM, no first- or second-degree relatives exhibit aura, including motor weakness [6]. SHM diagnosis is based on clinical findings and necessitates neuroimaging studies and lumbar puncture to exclude other causes. The current cases met the diagnostic criteria for SHM [6], and no abnormal findings were revealed on laboratory studies, brain MRI, MRA, or DW-MRI, except for cerebral hyperemia on SWI and 99mTc-HMPAO-SPECT studies. The mechanism of HM remains unclear and may or may not be the same as that of classic migraine. The previously accepted vascular theory attributes aura to transient ischemia caused by vasoconstriction and headache as due to rebound vasodilation of intracranial arteries. However, functional brain imaging during aura reveals spreading cortical hyperemia followed by oligemia [1]. The depolarization phase is linked to increased regional cerebral blood flow and positive symptoms (e.g., visual scintillation), followed by a phase of reduced neuronal activity associated with decreased regional cerebral blood flow and negative symptoms (e.g., visual scotoma) [1,2]. While migraine with aura and SHM exhibit similar clinical characteristics, the present patients experienced prolonged negative symptoms (hemiplegia, aphasia, hemineglect, and encephalopathy) associated with hyperemia of the unilateral hemisphere. Hyperperfusion of the hemisphere contralateral to the hemiparesis has been previously reported in patients with FHM. Oberndorfer et al. [5] found that perfusion MRI and SPECT showed hyperperfusion in the affected hemisphere of a patient with FHM, while DW-MRI results were normal. Lindahl et al. [4] reported increased perfusion in the unilateral hemisphere on perfusion MRI in patients with prolonged hemiplegia. Hsu et al. [3] demonstrated hyperemia and dilation of the intracranial arteries of the affected hemisphere on MRA, perfusion MRI, and CT angiography in patients with HM; their study also indicated the beneficial effect of verapamil on headache, but not on hemiplegia. SWI is a high-spatial-resolution three-dimensional gradient echo MR technique that exploits the magnetic susceptibility differences of various tissues, such as blood products (deoxyhemoglobin and methemoglobin), iron, and calcification. SWI comprises magnitude and phase images. A phase mask is created from the phase images and then multiplied by the magnitude images to accentuate the conspicuity of blood products and other sources of susceptibility effects [7,8]. SWI has been reported to be highly sensitive in vein detection [9,10], making it a suitable modality for demonstrating venous structures. In the present SHM cases, prolonged encephalopathy and hemiplegia were associated with contralateral cerebral hyperemia, which was confirmed using SWI and 99mTc-HMPAO-SPECT studies. SWI has rarely been employed as a diagnostic tool for HM. Although not yet widely used for diagnosing headaches, SWI can provide valuable additional information for evaluating HM.