|
 |
- Search
| Ann Child Neurol > Volume 31(3); 2023 > Article |
|
Abstract
Purpose
The present study investigated the clinical profile of children with primary headache at a tertiary care center in North India.
Methods
A retrospective observational study was conducted between January 2021 and October 2022. In total, 100 children 5 to 18 years of age who attended the pediatric outpatient department or the emergency department with primary headache were included. Children with secondary causes of headache were excluded.
Results
This study included 100 children (40 boys, 60 girls), and the female-to-male ratio was 1.5:1. The patients ranged in age from 5 to 18 years (mean±standard deviation, 10.1±2.8). Migraine headaches were most commonly reported (60%) followed by tension-type headache (28%) and others (12%). The throbbing type of pain was most common (43%), followed by the tightening type in 32%. The pain location was bilateral frontal in 47% of patients, followed by bitemporal in 20% and occipital in 17%. Most of the children (87%) had a headache duration of 2 to 4 hours. The common precipitating factors were skipped meals (25%), bright light (18%), lack of sleep (16%), and schoolwork (15%). A family history was present in around 62%. Around 70% of children required prophylactic medications (flunarizine and propranolol). Long screen time (2 to 4 hours/day) and a family history of headache were significantly associated with primary headache (P<0.05).
Headache is the most common neurological symptom manifesting as pain in childhood [1,2]. The diverse causes, frequency, and intensity of headache have a major impact on children’s intellectual performance, memory, personality, and school attendance [3-5]. Healthcare providers should be able to differentiate between primary and secondary headaches so that more sinister causes can be treated as early as possible, thus improving quality of life and minimizing disability [6]. The frequency of headache increases with age, and the underlying causes range from migraine and tension-type headaches (TTH) to life-threatening infections and brain tumors [7]. The reported prevalence of primary headache is 10% to 20% in school-aged children [8,9] and >50% in those under 20 years of age [10]. Data on pediatric headache in India are limited to a few school-based questionnaire surveys [11,12], case series of specific primary headaches, or isolated case reports of rare headache types [11]. Most childhood headaches are due to a primary headache disorder, such as migraine, or an acute benign process, such as viral infection. However, more serious causes of headache should always be ruled out [13]. Migraine remains the most common type of pediatric headache disorder, for which caregivers seek doctors’ opinions. A detailed evaluation of headache in the pediatric population is necessary for proper diagnosis and management.
The present study aimed to investigate the clinical profile and factors associated with primary headache in children at a tertiary care center in North India.
A retrospective, observational study was conducted at a tertiary care center in North India from January 2021 to October 2022. Children between 5 and 18 years of age who attended the pediatric outpatient department or the emergency department with primary headache were included in the study. Children presenting with headache due to fever, trauma, and/or other obvious causes, such as meningitis, dental conditions, and sinusitis, were excluded. This study was approved by the Institutional Review board of Command Hospital, Chandimandir (letter no. 14/03/CHWC/2022). The written informed consent by the patients was waived due to a retrospective nature of our study.
Children between the ages of 5 and 18 years with headache who visited the pediatric outpatient department or the emergency department of the hospital from January 2021 to October 2022 were identified using the hospital case sheets. The medical records of all these children were reviewed, and patients with primary headache whose records were complete were included in the current study. Children with diseases that could potentially be associated with secondary headache, such as brain tumors, sinus infections, dental related disease, febrile illness, other systemic diseases, and eye problems were excluded. Patients’ data were evaluated based on the medical records from the first visit. The diagnosis and classification of headache followed the International Classification of Headache Disorders (ICHD-3) beta version criteria applied to children and adolescents. We divided headaches into three groups: migraine, TTH, and other causes of headache. The documented patients’ data included demographic profile (such as age and sex) and clinical information (such as the location of the headache, character, duration, frequency, precipitating factors, family history, prophylactic medications, screen time), and headache severity (using a visual analogue scale in patients over 6 years of age and a face pain scale for children less than 6 years of age). The investigations included detailed eye evaluation, neuroimaging, electroencephalogram (EEG), and the house-tree-person (HTP) psychological test for any stressors. Data from all 100 children were noted in a Microsoft Excel spreadsheet (Microsoft Corp., Redmond, WA, USA) and analyzed for predefined variables.
The collected data were recorded in a Microsoft Excel spreadsheet. The statistical analysis was performed using SPSS version 20 (IBM Corp., Armonk, NY, USA). Categorical variables were presented as number and percentage, while continuous variables were presented as mean and standard deviation. The chi-square test was used to assess the associations of categorical variables with recurrent headache. A P value <0.05 was considered statistically significant.
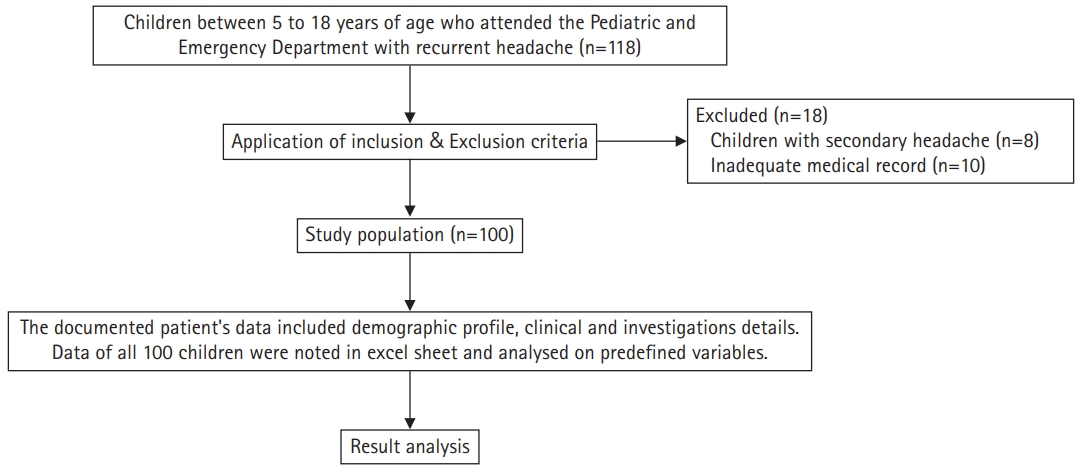
During the study period, 118 children presented with headache, of whom 18 were excluded from the study. Ten of them did not have appropriate medical records, while eight of them had secondary headache. The study flow is depicted in Fig. 1. The demographic data and clinical data are depicted in Tables 1 and 2, respectively. They ranged in age from 5 to 18 years (mean±standard deviation, 10.1±2.8). Boys (40/100) and girls (60/100) were distributed at a ratio of 1:1.5. Sixty percent of the patients had migraine (60/100), while 28% of the patients had TTH. The frontal location predominated in both groups, with a higher proportion in the migraine group (55%, 33/60) than in the TTH group (35.7%, 10/28). The most common character of the headache was throbbing in all three groups (P<0.05). The proportion ranged from 32.1% (9/28) in the TTH group to 66.7% (8/12) in the “others” group. The duration of headache in most patients was between 2 and 4 hours. The proportion of patients with headache lasting more than 4 hours was only 18.3% (11/60) in the migraine group and 7.2% (2/28) in the TTH group. The frequency of headache was either weekly or monthly in the majority of the patients. Various precipitating factors were found. Missing meals was the most common precipitating factor for headache in all three groups. Other common precipitating factors were family issues related to stressors in studies, academic difficulties, bright light, specific food items, sleep deprivation, and others. Almost half of the patients with migraine (25/60) scored the severity of their headache in the range of 3 to 5, while most patients with TTH scored their headache in the range of 6 to 8 (18/28). As far as the screen time was concerned, 58.3% of the children with migraine reported screen time of 2 to 4 hours. Most of the children with TTH reported screen time of either less than 2 hours (10/28) or more than 4 hours (10/28).
Neuroimaging was not done in nearly half the patients in the migraine and TTH groups. However, 66% of the children who were categorized under “others” were advised to undergo brain magnetic resonance imaging and all the patients had normal neuroimaging. Among the patients who underwent neuroimaging, the proportion of children with non-specific white matter signal changes was 26.7% and 14.3% in the migraine and TTH groups, respectively. The eye evaluation and EEG study were normal in the majority of patients in all three groups. The children with abnormal EEG findings never had seizure episodes. The HTP test revealed stressors in 41.7%, 35.8%, and 16.7% of patients in the migraine, TTH, and others groups, respectively. A positive family history of primary headache was found in 75% of the patients in the migraine group, while the proportion was 53.6% in the TTH group (Table 3). Screen time, family history, and pain character were the only factors significantly (P<0.05) associated with primary headache (Table 3).
Headache has a major impact on children’s intellectual performance, memory, personality, and activities of daily living. Very scant literature is available on the prevalence of pediatric headache in India and the factors responsible for recurrence of primary headache. Questionnaire-based studies provide more reliable information and are feasible, yet clinical interviews are the gold standard for such studies [8]. In our study, we retrospectively analyzed the clinical data of children with recurrent headache. Similar to the existing literature [8,10,11], we observed that the prevalence of headache was higher in girls than in boys. Both migraine and TTH were found to be more common in girls.
In our study, the prevalence of migraine was 60% and TTH was 28% among children presenting with complaints of recurrent headache. These prevalence rates were much higher than those of 6% to 10% for migraine and 15% to 18% for TTH reported in previous studies, with migraine being the common sub-type of headache in children, followed by TTH [13-15]. The wide variation in the prevalence rates could be because those studies involved questionnaires administered to all school-going children, while ours is based on the retrospective analysis of clinical data of children presenting with headache in our clinical setting. The variation also could be because our study was conducted in different geographical region from the previous studies. The disparity in the prevalence rates could be due to ICHD-3 definitions used in our study, which were not used in the previous studies, which were conducted prior to the implementation of the ICHD-3 criteria. However, a questionnaire-based Indian study by Gupta et al. [8] conducted among school-going children showed a high prevalence of both migraine and TTH, with migraine being more common than TTH, similar to our findings. In most of the children, the headache was localized to the frontal region in both migraine and TTH, contrary to the general view of a “constricting band”-like diffuse headache in TTH.
Not many studies have compared the precipitating factors of migraine and TTH in children [16]. In our study, we found that hunger (“skipping meals”) was a common precipitating factor for both the types of headaches. This underlines the need to focus on educating children and parents about maintaining a healthy lifestyle with timely meals. Although in the current study, we did not focus on studying the effect of education of parents on the recurrence of headache episodes, the current findings suggest that further studies are required on this topic. In our study, we also observed that presence of a positive family history predisposed children to recurrent episodes of headache, especially in cases of migraine rather than TTH, similar to previous studies, indicating the presence of an underlying genetic predisposition in the pathophysiology of headaches.
Our findings in this study are in agreement with previous research in children and adolescents, which observed a relationship between screen time exposure and migraine in those using digital/electronic gadgets routinely [17]. We observed that more than half of the children with migraine had a large amount of screen time (2 to 4 hours). Although we do not have direct insights into the biological basis, it has been hypothesized that the luminosity or frequency of the screen’s light might directly trigger an acute attack of migraine [18]. According to previous studies, no markers have yet been identified that can predict the recurrence of headache in children. A recent study by Lund et al. [19] showed that more screen time was associated with more frequent headaches in children, but the causality of this association was not established. However, in this study, we observed that screen time could be used as a surrogate marker for predicting the recurrence of headache, more so in children with migraine than in those with TTH and other types of headaches. However, larger studies are warranted to substantiate these findings. Nevertheless, focus should be given to highlighting the importance of optimizing the screen time and establishing appropriate etiquette for using screen-based gadgets.
The HTP projective drawing test provides clinically meaningful information regarding an individual’s psychological, emotional, and mental health condition. Although a recent study by Lin et al. [20] cast doubt on the validity of the HTP test in predicting mental health, this test has long been used for identifying stressors with good reliability. In our study, the HTP test identified the presence of stressors not only in those with migraine, but also in those with TTH and other forms of headaches.
In conclusion, primary headache disorders were more common than secondary headache, with migraine being the commonest type observed. Headache prevalence increased with increasing age, and girls were more often affected than boys. Prospective studies involving a larger number of children are further warranted. In addition, reducing screen time and not skipping meals should be encouraged for all children with primary headaches.
Notes
Author contribution
Conceptualization: RS and DS. Data curation: RS and AU. Formal analysis: GK and SS. Methodology: RS and AU. Visualization: SS. Writing-original draft: RS. Writing-review & editing: GK and SS.
Table 1.
Patients’ demographic and clinical characteristics
| Characteristic | Migraine (n=60) | Tension-type headache (n=28) | Others (n=12) | P valuea |
|---|---|---|---|---|
| Age (yr) | 10.9±2.7 | 9.7±2.6 | 6.9±1.3 | |
| Sex | 0.37 | |||
| Male | 27 (45) | 10 (35.7) | 3 (25) | |
| Female | 33 (55) | 18 (64.3) | 9 (75) | |
| Location | 0.06 | |||
| Frontal | 33 (55) | 10 (35.7) | 4 (33.3) | |
| Temporal | 9 (15) | 6 (21.4) | 5 (41.7) | |
| Occipital | 6 (10) | 8 (28.6) | 3 (25) | |
| Diffuse | 8 (13.3) | 1 (3.6) | 0 | |
| Unilateral | 4 (6.7) | 3 (10.7) | 0 | |
| Character | 0.01 | |||
| Throbbing | 26 (43.3) | 9 (32.1) | 8 (66.7) | |
| Tightening | 13 (21.7) | 15 (53.6) | 4 (33.3) | |
| Pricking | 13 (21.7) | 4 (14.3) | 0 | |
| Undefined | 8 (13.3) | 0 | 0 | |
| Duration of pain (hr) | 0.21 | |||
| 1-2 | 24 (40) | 12 (42.8) | 8 (66.7) | |
| 2-4 | 25 (41.7) | 14 (50) | 4 (33.3) | |
| >4 | 11 (18.3) | 2 (7.2) | 0 | |
| Frequency | 0.91 | |||
| Daily | 12 (20) | 4 (14.3) | 2 (16.7) | |
| Weekly | 22 (36.7) | 13 (46.4) | 5 (41.7) | |
| Monthly | 21 (35) | 9 (32.1) | 3 (25.0) | |
| 3-monthly | 5 (8.3) | 2 (7.2) | 2 (16.6) | |
| Precipitating factors | 0.79 | |||
| Family issues | 3 (5) | 1 (3.6) | 2 (16.7) | |
| Lack of sleep | 10 (16.7) | 4 (14.3) | 2 (16.7) | |
| Academic issues | 9 (15) | 5 (17.8) | 1 (18.2) | |
| Missing meals | 16 (26.7) | 6 (21.4) | 3 (25) | |
| Bright light | 9 (15) | 7 (25) | 2 (16.7) | |
| Food-related | 6 (10) | 1 (3.6) | 2 (16.7) | |
| No factor | 7 (11.6) | 4 (14.3) | 0 | |
| Headache severity scoreb | 0.08 | |||
| <3 | 10 (16.6) | 3 (10.7) | 3 (25) | |
| 3-5 | 25 (41.7) | 4 (14.3) | 6 (50) | |
| 6-8 | 19 (31.7) | 18 (64.3) | 3 (25) | |
| 9-10 | 6 (10) | 3 (10.7) | 0 | |
| Screen time (hr) | 0.02 | |||
| <2 | 10 (16.7) | 10 (35.7) | 5 (41.7) | |
| 2-4 | 35 (58.3) | 8 (28.6) | 2(16.6) | |
| >4 | 15 (25) | 10 (35.7) | 5 (41.7) | |
| Family history | 0.04 | |||
| Yes | 45 (75) | 15 (53.6) | 2 (16.7) | |
| No | 15 (25) | 13 (46.4) | 10 (83.3) |
Table 2.
Investigations and treatment characteristics
| Variable | Migraine (n=60) | Tension-type headache (n=28) | Others (n=12) | P valuea |
|---|---|---|---|---|
| Neuroimaging (CT/MRI) | 0.06 | |||
| Normal | 17 (28.3) | 12 (42.8) | 8 (66.7) | |
| Abnormal | 16 (26.7) | 4 (14.3) | 0 | |
| Not done | 27 (45) | 12 (49.1) | 4 (33.3) | |
| Eye evaluation | 0.71 | |||
| Normal | 49 (81.7) | 24 (85.7) | 9 (75) | |
| Abnormal | 11(18.3) | 4 (14.3) | 3 (25) | |
| Electroencephalography | 0.51 | |||
| Normal | 51(85) | 25 (89.2) | 10 (83.3) | |
| Abnormal | 9 (15) | 3 (10.8) | 2 (16.7) | |
| Background irregularity | 5 | 1 | 1 | |
| Epileptiform discharge | 3 | 1 | 1 | |
| Paroxysmal activity | 1 | 1 | 0 | |
| House-tree-person test for stressors | 0.25 | |||
| Stressors not present | 35 (58.3) | 18 (64.2) | 10 (83.3) | |
| Stressors present | 25 (41.7) | 10 (35.8) | 2 (16.7) | |
| Prophylactic medications | 0.42 | |||
| Yes | 39 (65) | 21 (75) | 10 (83.3) | |
| No | 21 (35) | 7 (25) | 2 (16.7) | |
Table 3.
Important factors associated with primary headache
| Factor | Migraine (n=60) | TTH (n=28) | Others (n=12) | P valuea |
|---|---|---|---|---|
| Screen time (hr) | 0.02 | |||
| <2 | 10 (16.7) | 10 (35.7) | 5 (41.7) | |
| 2-4 | 35 (58.3) | 8 (28.6) | 2 (16.6) | |
| >4 | 15 (25) | 10 (35.7) | 5 (41.7) | |
| Family history | 0.04 | |||
| Yes | 45 (75) | 15(53.6) | 2 (16.7) | |
| No | 15 (25) | 13(46.4) | 10 (83.3) | |
| HTP test for stressors | 0.25 | |||
| Absent | 35 (58.3) | 18 (64.2) | 10 (83.3) | |
| Present | 25 (41.7) | 10 (35.8) | 2 (16.7) | |
| Character of pain | 0.01 | |||
| Throbbing | 26 (43.3) | 9 (32.1) | 8 (66.7) | |
| Tightening | 13 (21.7) | 15 (53.6) | 4 (33.3) | |
| Pricking | 13 (21.7) | 4 (14.3) | 0 | |
| Undefined | 8 (13.3) | 0 | 0 |
References
1. Kernick D, Campbell J. Measuring the impact of headache in children: a critical review of the literature. Cephalalgia 2009;29:3-16.


3. Pascual J. Prevalence of primary headaches: it is not the behavior, but still we have to pay attention to it! J Headache Pain 2011;12:139-40.




4. Parisi P, Vanacore N, Belcastro V, Carotenuto M, Del Giudice E, Mariani R, et al. Clinical guidelines in pediatric headache: evaluation of quality using the AGREE II instrument. J Headache Pain 2014;15:57.
5. Lopez JI, Bechtel KA, Rothrock JF. Pediatric headache [Internet]. New York: Medscape; 2017 [cited 2023 Feb 16]. Available from: https://emedicine.medscape.com/article/2110861


7. Gurkas E, Karalok ZS, Taskin BD, Aydogmus U, Yilmaz C, Bayram G. Brain magnetic resonance imaging findings in children with headache. Arch Argent Pediatr 2017;115:e349-55.


8. Gupta R, Bhatia MS, Dahiya D, Sharma S, Sapra R, Semalti K, et al. Recurrent headache in Indian adolescents. Indian J Pediatr 2009;76:733-7.



9. Shivpuri D, Rajesh MS, Jain D. Prevalence and characteristics of migraine among adolescents: a questionnaire survey. Indian Pediatr 2003;40:665-9.

10. Abu-Arafeh I, Razak S, Sivaraman B, Graham C. Prevalence of headache and migraine in children and adolescents: a systematic review of population-based studies. Dev Med Child Neurol 2010;52:1088-97.


11. Chakravarty A. Chronic daily headache in children and adolescents: a clinic based study from India. Cephalalgia 2005;25:795-800.



12. Mishra D, Choudhury KK, Gupta A. Headache with autonomic features in a child: cluster headache or contact-point headache? Headache 2008;48:473-5.


13. Mavromichalis I, Anagnostopoulos D, Metaxas N, Papanastassiou E. Prevalence of migraine in schoolchildren and some clinical comparisons between migraine with and without aura. Headache 1999;39:728-36.


14. Al Jumah M, Awada A, Al Azzam S. Headache syndromes amongst schoolchildren in Riyadh, Saudi Arabia. Headache 2002;42:281-6.


15. Lu SR, Fuh JL, Juang KD, Wang SJ. Migraine prevalence in adolescents aged 13-15: a student population-based study in Taiwan. Cephalalgia 2000;20:479-85.



16. Robbins L. Precipitating factors in migraine: a retrospective review of 494 patients. Headache 1994;34:214-6.


17. Montagni I, Guichard E, Carpenet C, Tzourio C, Kurth T. Screen time exposure and reporting of headaches in young adults: a cross-sectional study. Cephalalgia 2016;36:1020-7.



18. Kowacs PA, Piovesan EJ, Werneck LC, Fameli H, Pereira da Silva H. Headache related to a specific screen flickering frequency band. Cephalalgia 2004;24:408-10.