Orbital Myositis Mimicking Status Migrainosus
Article information
Idiopathic orbital myositis is a primary inflammatory disease involving the extraocular muscles that is currently classified as a subcategory of idiopathic orbital inflammatory syndrome [1]. It is typically characterized by the sudden onset of pain and other inflammatory signs such as edema and erythema in the periorbital area. Although it accounts for 6.3% of all orbital diseases in adults [2], its incidence among children is very low and only a single case has been reported in the past decade in South Korea [3]. Pediatric orbital myositis differs from its adult counterpart in that it is characterized by a bilateral manifestation with constitutional symptoms such as headache [4,5]. This makes it difficult for clinicians to include orbital myositis in the differential diagnosis when a child presents with headache at the beginning of the clinical course. Herein, we report the case of an adolescent girl with orbital myositis whose first presentation was recurrent headache without any neurological abnormalities.
A 17-year-old female patient visited the emergency room with a complaint of persistent headache in the left temporal area. She had experienced throbbing headaches for 5 to 6 years, twice a month, mainly in the daytime. Each headache would gradually start as a feeling of tightness in the left temporal area, and then spread to include the entire head. Her condition was relieved within an hour by taking paracetamol. However, at the time of her visit, the acute attack was persistent and disabling and accompanied by nausea, vomiting, and dizziness.
The physical examination, neurological examination, visual acuity test, and fundoscopy were assessed as normal. The complete blood test panel, erythrocyte sediment rate, and C-reactive protein levels showed normal findings. The patient was first diagnosed with an acute migraine attack and admitted for an acute treatment plan and a preventive treatment plan.
There was no reduction in the severity, duration, and frequency of headaches, and the patient complained of diplopia on the next day. Thorough physical and neurological examinations were repeated. We found that there was a subtle restriction of the outward movement of the left eye. The patient complained of diplopia and pain when gazing to the left during the examination. Mild swelling on the left periorbital area was also noticed. Fundoscopy revealed a normal optic disc and flat posterior pole.
The findings of diplopia and extraocular movement limitations warranted neuroimaging, and the patient underwent brain magnetic resonance imaging (MRI). High signal intensity in the left medial rectus muscle on T2-weighted images was noticed. The patient underwent orbital MRI for further investigation, which disclosed high signal intensity and thickening in the left medial rectus muscle, involving the tendon on fat-saturated T2-weighted images (Fig. 1A) and gadolinium enhancement on T1-weighted images (Fig. 1B). The findings were suggestive of myositis of the left medial rectus muscle. Thyroid hormones and antibodies, as well as acetylcholine receptor antibody levels, were assessed for the differential diagnosis, and the patient was diagnosed with idiopathic orbital myositis.
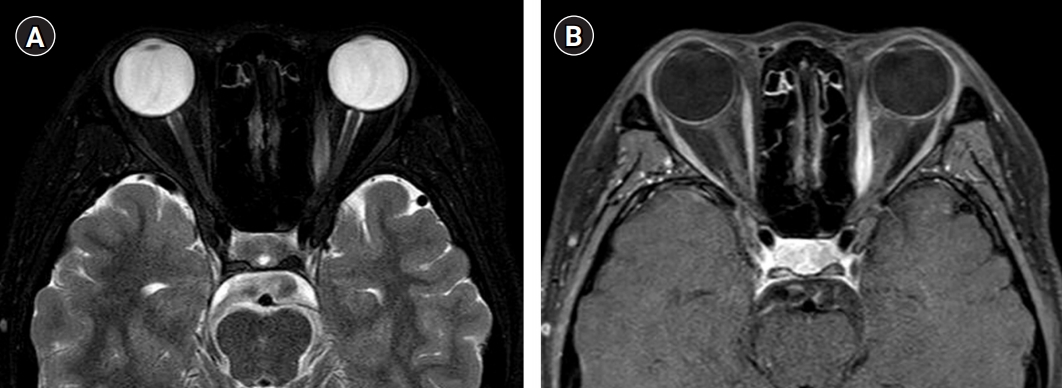
(A) Fat-saturated T2 shows increased signal intensities and thickening of the left medial rectus, axial view. (B) Gadolinium enhancement of left medial rectus muscle in T1-weighted, axial view.
The patient was started on oral prednisone at 1 mg/kg/day for 3 weeks. Marked pain relief was noted within 2 days and the findings of diplopia and extraocular movement limitations were completely ameliorated after 10 days. The treatment was followed by gradual tapering of steroids over 12 weeks. Follow-up orbital MRI was performed after 12 weeks of treatment and displayed a reduction in the diameter and signal intensity of the left medial rectus muscle. She remained clinically stable without recurrence.
Orbital myositis is a subcategory of idiopathic orbital inflammatory syndrome, which is the most common cause of painful orbital masses in adults [1,2]. Pediatric orbital myositis is extremely rare. There have been 12 reported cases of orbital inflammatory syndrome in a 6-year period, and only one case was orbital myositis [5]. One case of pediatric orbital myositis has been reported in Korea, after alloplastic implant insertion in a blow-out fracture [3]. In addition to its rarity, pediatric orbital myositis is a challenging disease to diagnose because of its constitutional symptoms, bilaterality, and recurrence [4,5]. Because other ocular presentations such as proptosis, conjunctival injection, chemosis, periorbital area, and diplopia can be absent in pediatric patients, it is easy for physicians to misdiagnose orbital myositis as primary headache at the beginning of the disease course [6]. The differential diagnosis of orbital myositis includes orbital infections, thyroid-associated orbitopathy, lymphoma, systemic lupus erythematosus, myasthenia gravis, diabetes, immunoglobulin G4-related ophthalmic disease, Tolosa-Hunt syndrome, ophthalmoplegic migraine, optic neuritis, and carotid cavernous fistula [7-9].
The most sensitive diagnostic tool to diagnose orbital myositis is orbital MRI. Typical findings of orbital myositis include signal enhancement and thickening in the involved extraocular muscles, including the myo-tendinous junction on fat-saturated T2-weighted images, as shown in this patient [6].
Although the etiology of idiopathic orbital myositis is unknown and continues to be investigated [10], steroids are well tolerated and show marked clinical improvement within a few days in most patients, as in this case. The dose of corticosteroid ranges from oral prednisone (1 mg/kg/day for 2 weeks, and gradual tapering over more than 4 weeks) to intravenous methylprednisolone (500 to 1,000 mg/day) [7,8]. If patients show no clinical resolution or worsening symptoms, immuno-suppressants such as cyclosporine A, cyclophosphamide, methotrexate, mofetil mycophenolate, rituximab, and radiotherapy are warranted [7,8].
The diagnosis was challenging in our case because the patient complained of headache at the first visit without ocular symptoms, such as exacerbation of orbital pain when moving, which is the cardinal clinical feature of orbital myositis. This underscores the importance of repeated and thorough neurological examinations in patients with worsening headaches. Physicians should take orbital myositis into consideration when a patient with headache complains of symptoms involving the eyes. A prompt recognition of newly developed symptoms and signs can help minimize the disability of pediatric orbital myositis patients since oral corticosteroids can easily lead to symptom resolution within a few days.
Written consent to publish this report was obtained from the patient. This study was approved by the Institutional Review Board (IRB) of the St. Vincent’s Hospital (No. VC19ZASI0273).
Notes
No potential conflict of interest relevant to this article was reported.
Author contribution
Conceptualization: IHY. Data curation: IHY. Formal analysis: IHY. Methodology: YJK and IHY. Project administration: YJK and IHY. Visualization: YJK. Writing-original draft: YJK. Writing-review & editing: YJK and IHY.
