Factitious Seizures and Limb Paralysis in Munchausen Syndrome
Article information
Munchausen syndrome is a rare factitious disorder, characterized by either the intentional manifestation of physical symptoms or repeated self-injuries in order to achieve health care attention, complemented by pathological lying and a restless wandering from hospital to hospital for medical and/or surgical interventions [1]. Along with wounds and psychic symptoms, one of the commonest presenting complaint is seizures [2]. Here, we document an interesting case, presenting as factitious psychogenic nonepileptic paroxysmal episodes and limb paralysis.
An 18-year-old male visited the emergency room (ER) with postictal limbs paralysis. Witnesses reported that he suffered a generalized tonic seizure-like event, followed by paraplegia or quadriplegia on resumption of consciousness. Social history revealed that his parents divorced when he was 8 years old and he was subsequently raised by his grandmother. From 9 years of age, he frequently visited ER for varying complaints, including lower extremity arthralgia, chest palpitation, and dyspnea. However, investigations did not show any abnormality. Past surgical history consisted of three episodes of orthopedic surgery and an appendectomy with a grossly normal appendix. He developed his first paroxysmal behavior at the age of 13. While the clinical semiology was bizarre, with brief tremulous movements and the absence of drooling or lip cyanosis, his brain magnetic resonance imaging (MRI) and interictal electroencephalography (EEG) were normal. The caregiver always described it like convulsion and was overly concerned about the child's strange appearance. So we were forced to start epilepsy treatment. Not surprisingly we unsuccessfully tried several anticonvulsants. Because of repeated episodes and need for active management, he was eventually received the vagus nerve stimulation therapy.
Interestingly, he also experienced several episodes of lower extremity paralysis after seizure-like event, from which he miraculously recovered without any lingering neurologic deficit. A wide array of tests was frequently done, including spinal cord MRI, cerebrospinal fluid analysis, motor and somatosensory evoked potential test, and nerve conduction study. While the patient reported limb paralysis, none of the results were abnormal.
Currently, we performed continuous video EEG monitoring, in anticipation of a seizure. However, he showed non-epileptic behaviors, without suspicious EEG changes (Fig. 1). More importantly, he was discharged 1 hour later, without any neurologic deficit. Eventually, the anticonvulsants was reduced, and neuropsychiatry clinic was recommended. He never visited our hospital again. His recurrent episodes of simulation of epileptic attacks with limb paralysis and rapid recovery, in the presence of normal investigations, were highly suggestive of Munchausen syndrome.
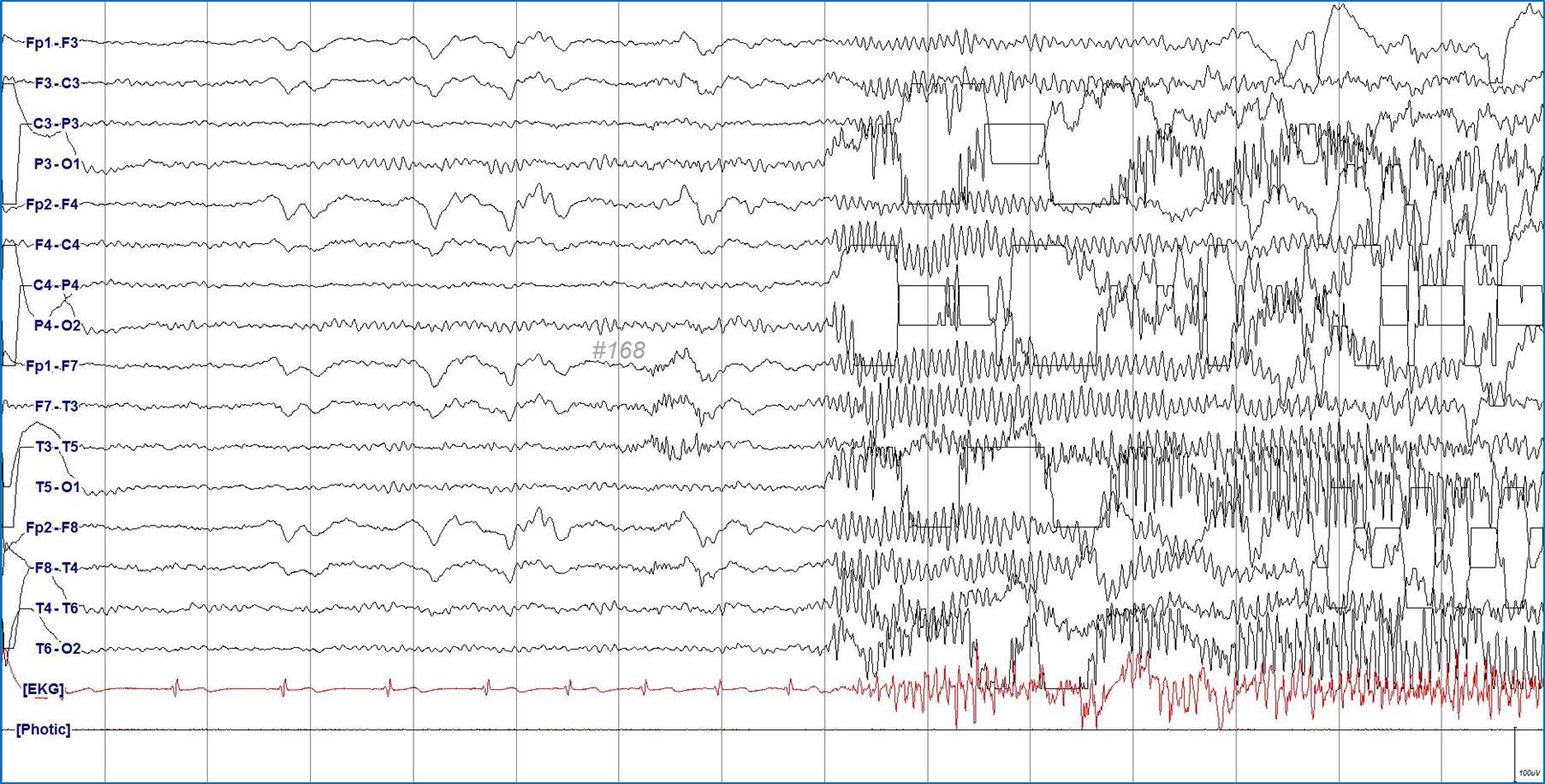
Electroencephalography (EEG) finding during habitual ictal event. He showed generalized tremulous movements lasting for 10 seconds but simultaneous EEG revealed bitemporally dominant fast activities without true epileptiform discharge.
Patients with Munchausen syndrome have an underlying desire for attention, sympathy, compassion, and in some cases addictive medicine, invasive examinations and operations [3,4]. Even in the absence of obvious external rewards from their behavior, they just satisfy with the sick role. While their motivation is frequently unknown, some psychosocial features such as early losses via death, sickness, or abandonment; disrupted attachments to others due to neglect, abuse, or other traumas; are usually common in patients with the disorder [4,5]. Therefore, early diagnosis is important and requires the systematic collection of relevant information, including a detailed chronology of the patient’s past medical history and a careful scrutiny of his medical record. Moreover, a supportive relationship has to be established with the patient and his family in order to increase compliance to psychotherapy. It is important that epileptologists keep Munchausen syndrome as part of their differential diagnosis in patients presenting with an unusual seizure semiology or medical history. In such cases, shor-term video EEG monitoring with verbal suggestion is a useful and cost effective diagnostic test.
Notes
No potential conflict of interest relevant to this article was reported.
Author contribution
Conceptualization: WSK. Supervision: WSK. Investigation: JSK. Visualization: JSK. Writing: JSK.
