The First Case Report of Neonatal Bacterial Meningitis Caused by Streptococcus alactolyticus
Article information
Streptococcus alactolyticus is grouped in S. bovis/S. equinus complex (SBSEC). SBSEC is found in the intestinal flora of humans and animals [1]. Certain bacteria include in SBSEC have caused human infection such as bacteremia or meningitis, but S. alactolyticus was identified rarely as pathogen in a few case. Especially, only one case was reported in neonatal sepsis. A case of fatal neonatal sepsis without meningitis due to S. alactolyticus has been reported, but the pathogen was identified in gastric fluid and samples from ear, trachea, and nasopharynx, not in blood and cerebrospinal fluid (CSF) [2]. Until now, there was no case report that was culture-proven S. alactolyticus as pathogen of neonatal bacterial meningitis. This is the first case presenting neonatal bacterial meningitis and sepsis caused by S. alactolyticus and treated successfully.
A 28-day-old baby girl presented to our hospital with 2 day-fever history. She was born at 36 weeks and 2 days of gestational age, weighing 2,800 g by cesarean section. There were no prenatal and perinatal problems. After birth, she was healthy, fed well and had been cared-for at home. She got hepatitis B vaccination at birth.
Examinations on other hospital revealed a fever, heart rate, and respiration rate of 38.7℃, 168 beats/min, and 44/min, respectively. There were no abnormal sign on physical examination. Specimens for laboratory studies and blood, urine, and CSF cultures were collected. Intravenous ampicillin and cefotaxime were administered. Laboratory analysis results are shown in Table 1. Four hours later after spinal tapping, she was transferred to our institution. On the first admission day, only blood test was done, and the results are shown in Table 1. We administered vancomycin instead of ampicillin and cefotaxime without spinal tapping because she was 4 weeks old. She had high fever up to 39℃ every 6 hours. On day 3, a second blood sampling and lumbar puncture was performed, and the results described in Table 1. The FilmArray Meningitis/Encephalitis polymerase chain reaction panel (BioFire Diagnotics, Salt Lake City, UT, USA) revealed no pathogen. We were notified that there were gram-positive cocci on the Gram stain of CSF from the previous hospital. We then administered ampicillin. And we also added acyclovir because we could not exclude herpes infection. However, the fever lasted, and the patient looked acutely ill. To rule out complications, brain magnetic resonance image and electroencephalography were performed, and this showed no specific abnormality. There was no fever any more after hospitalization day 4. On day 5 the results of CSF and blood culture, which were performed at the previous hospital, were obtained. S. alactolyticus was isolated from the blood and CSF and susceptible to ampicillin (minimum inhibitory concentration ≤0.25) (Table 2). Vancomycin, cefotaxime and acyclovir were discontinued, leaving only ampicillin to be administered. A second CSF and blood culture examination performed in our hospital showed no growth of any pathogen. After completing a 14-day course of intravenous ampicillin, she showed improvement and was discharged without any complications. She has subsequently been followed up for developmental assessment and hearing tests for over 2 months. The hearing test results were normal, and she shows normal development for her age.
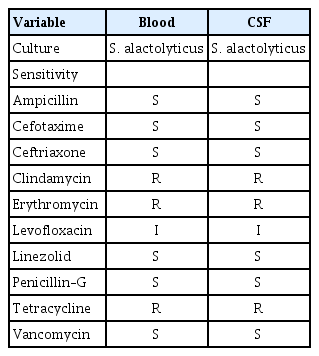
Results of the culture and antibiotic sensitivity tests for blood and cerebrospinal fluid of the patient
Late onset meningitis in neonates is defined as meningitis occurring after 72 hours of birth and is predominantly seen in premature infants. The incidence is directly related to decreasing birth gestational age and weight. Coagulase-negative staphylococci and S. aureus are the common causative pathogens. After primary bacterial infection has occurred in bloodstream, the infection spreads through the systemic bloodstream. Bacteria in microvasculature of the central nervous system invade the CSF, causing an inflammation reaction, which results in meningitis. Therefore, neonatal meningitis is mostly concurrent with neonatal sepsis. However, it is possible to obtain a positive CSF culture although the blood culture is negative. This is because survivors of neonatal meningitis are more susceptible to developmental delay or neurologic sequelae; it is important and necessary to have prompt diagnosis and treatment of neonatal meningitis and regular follow-up about its development. Therefore, if there are clinically suspected sepsis or infection signs, CSF analysis and culture should be performed to identify the presence of meningitis.
SBSEC is found in the intestinal flora of humans and animals and is classified into four DNA homology clusters based on 16S ribosomal DNA [1,3]. S. alactolyticus, the only species in DNA cluster Ⅳ, were isolated exclusively from the intestine of pigs, chicken, pigeons, and canines. S. alactolyticus is an extremely rare causative pathogen of human infection [1]. Until now, only three cases of human infection are reported, and only one of them was neonatal sepsis [2]. A 65-year-old woman with a history of left ventricular outflow tract obstruction in hypertrophic cardiomyopathy was diagnosed as S. alactolyticus infective endocarditis which was complicated by septic emboli and mycotic left middle cerebral artery aneurysm [4]. A 35-year-old type 1 diabetic woman who presented with severe diabetic ketoacidosis, precipitated by S. alactolyticus bacteremia, was successfully treated [5]. Toepfner et al. [2] described neonatal fulminant sepsis caused by S. alactolyticus; a full-term infant that did not have any prenatal problem showed respiratory failure immediately after birth. Endotracheal intubation and mechanical ventilation were started, but the patient showed tachycardia, hypotension, and pulmonary hemorrhage. Despite appropriate treatment, the patient showed no in clinical symptoms and signs and died within 23 hours of life. S. alactolyticus was identified in the gastric and tracheal fluid of the patient but no pathogen was found in the blood and CSF [2].
To the best of our knowledge, this is the first case report that bacterial meningitis due to S. alactolyticus occurred in neonate without any history of animal contact and outdoor activities going out. Nevertheless, we could not find out the source of S. alactolyticus, the patient responded well to a 2-week course of ampicillin and was treated successfully. After discharge, she has been checked twice for 2 months in the outpatient clinic and there have been no complications, such as seizure, hearing loss or developmental delay.
Notes
No potential conflict of interest relevant to this article was reported.
Author contribution
Conceptualization : LY and YMK. Data curation : JKP. Writing-original draft : SJP. Writing-review & editing : LY and YMK.

